Do you worry about dying of rabies?
Preventive vaccination can protect you for the rest of your life against rabiesEveryone in Nepal should beware of dogs in the streets, which are the most likely source of rabies infection. Rabid dogs are not always aggressive. They can be partly paralysed and drooling saliva.
A bite, scratch or even licking an open wound by an unknown dog or any sick-looking mammal should be taken seriously. The best treatment following a dog bite is to wash the wound immediately with soap or detergent and then go to a hospital or clinic straight away for advice.
It is urgent to begin treatment if it is prescribed. A course of rabies vaccine is 3 or 4 doses, and an injection of rabies immune serum into the wound may be given if the risk is severe. Treatment is free in Nepal’s government hospitals and clinics, but the immune serum is expensive and only available at major hospitals.
Private clinics may provide treatment but at a cost. If this preventive treatment is delayed or is incomplete the risk of rabies infection remains. Treatment is most urgent if the bites are on the head, neck or hands.
Over 100 people die from rabies in Nepal every year, according to Hemant Ojha, head of zoonotic at Epidemiology and Diseases Control Division, and there are nearly 3 million dogs, many of them strays. More than 132,000 people were bitten by dogs andwild animals last year, and 40% of them were children.
This year alone, there have been about a dozen reported deaths already, and the government is trying to address the shortage of vaccines in hospitals around the country. However, pre-exposure vaccine before being bitten by a rabid animal is 100% effective.
Although rabies infection is 100% fatal once the illness has started, the vaccine can be 100% protective if given before contact with a rabid animal. No one has ever died of rabies who has had a course of pre-exposure vaccine and later, if bitten by a possibly rabid animal, had a booster vaccination. Rabies immune serum is not needed.
For pre-exposure vaccination, only a small amount of vaccine is needed and 0.1 ml can be injected into the surface of the skin. One vial of vaccine can be shared between a family or other group of people which reduces the cost.
A separate syringe and needle must be used for each person. However, they must all go to the clinic together because an opened vial must be discarded at the end of the day. A vial of vaccine costs approximately NPR 650–700 at pharmacies, private clinic charges vary. If bitten by an animal later in life, only booster vaccine is needed but rabies immune serum is not needed.
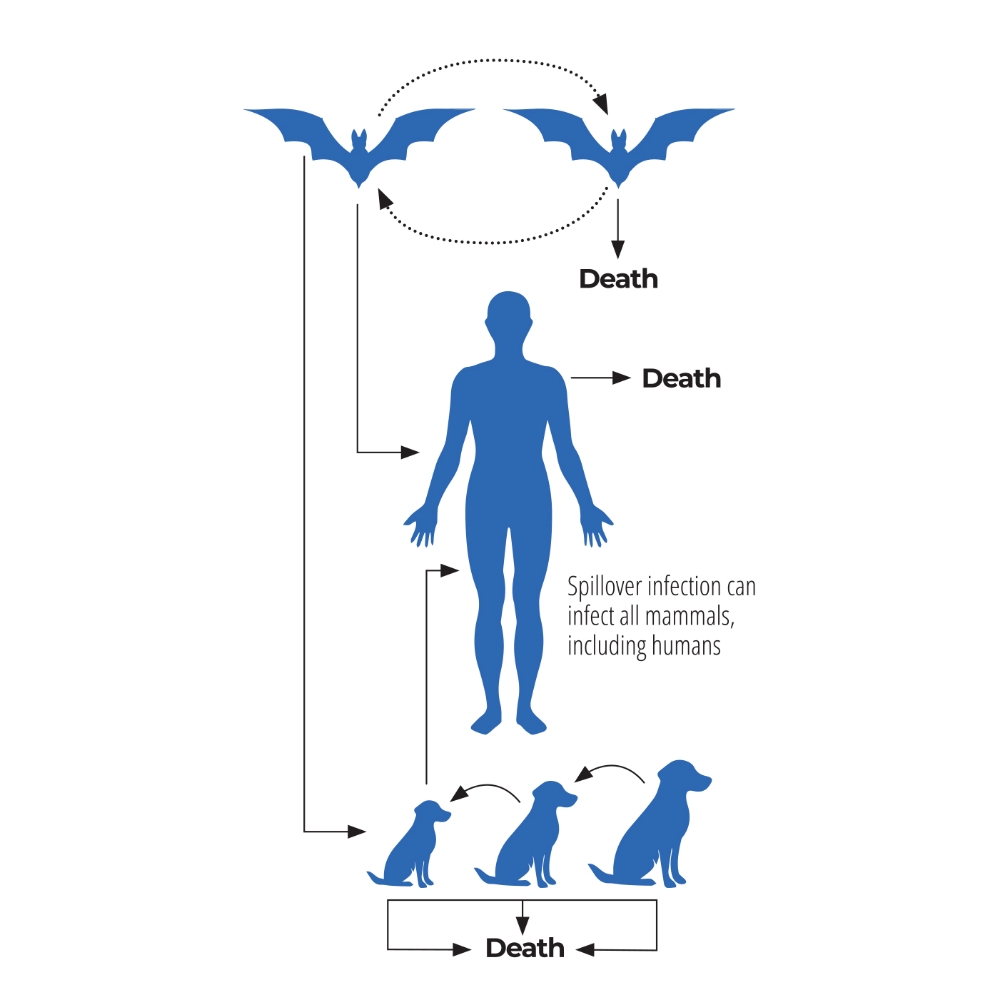
Only mammals can be infected by rabies, including dogs, cats, cattle, sheep, buffalo and wild mammals including bats. In humans many cases are not reported but a study in India showed that 12,700 people die of rabies every year. 40% of the deaths are in children under the age of 15 years.
Bites or even a scratch, usually from a rabid dog or cat, can result in an agonising death a few months later. The virus in the animal’s saliva is inoculated through the skin, and travels in nerves up to the brain. The rabies virus multiplies resulting in inflammation of the brain.
Read also: The return of communicable diseases, Sonia Awale
The diagnosis of rabies encephalitis depends on recognising the typical symptoms in people who have been in contact with a possibly rabid mammal in the previous weeks or months. The most characteristic symptoms are jerky muscle contractions, like quick gasps for air when trying to drink water, also fear of water, going on to fits, confusion and anxiety.
The infection progresses to unconsciousness, and breathing, heart or nervous system complications might follow. When the facilities exist, the possibility of giving intensive care to prolong life may arise, but although a very few patients, who have had incomplete vaccination, may survive a few weeks or months, they will be left with severe disability, unable to feed themselves, walk or talk.
Rabies infection can sometimes be a paralysing illness like polio, without spasms. When the muscles of breathing become paralysed, the patient dies. Tests on the patients’ skin or saliva can confirm the diagnosis, but this is not likely to be possible locally. After death a tiny sample of brain tissue can be tested.
In a disease as agonising and terrifying as rabies, relieving distressing symptoms is the primary concern. Because there is no treatment which will kill the virus in the brain, the only option is to give active compassionate care, to reduce suffering. Palliative therapy must reduce thirst and dehydration, fever, anxiety, fear, restlessness, agitation, seizures and pain.
The patient should be nursed in quiet darkened rooms, because bright lights and loud noises might provoke spasms. Fluids, sedatives and anticonvulsants help to keep the patient comfortable. Death usually occurs within a week or so.
In an ideal world, everyone in Nepal could have peace of mind by having a complete course of vaccine. Children are at greatest risk as they are less aware of rabies and may not report contact with a possibly rabid animal.
Mary Warrell was with the Centre for Clinical Vaccinology and Tropical Medicine, University of Oxford.




